Vital pulp therapy: an evidence-based approach to preserving tooth vitality
Vital pulp therapy (VPT) comprises biologically based procedures designed to preserve the vitality of the dental pulp following carious, traumatic, or iatrogenic exposures. By maintaining the pulp’s defense and regenerative potential, VPT contributes to tooth longevity and reduces the need for more invasive treatment. Recent advances in pulp biology, bioactive materials, and clinical protocols have significantly improved treatment predictability, leading to broader acceptance of VPT in daily practice.
Biological principles
The dental pulp is a dynamic tissue capable of healing and regeneration. Following injury, it can mount an inflammatory response, recruit progenitor cells, and stimulate reparative dentinogenesis, provided contamination is prevented. Successful VPT depends on:
-
Accurate pulpal diagnosis (reversible vs. irreversible pulpitis)
-
Control of inflammation and infection
-
Use of bioactive capping materials to promote healing and mineralization
-
A hermetic coronal seal to prevent bacterial ingress
Clinical indications
VPT can be considered when:
-
the pulp remains vital despite exposure (carious, traumatic, or iatrogenic)
-
signs and symptoms indicate a healthy or reversibly inflamed pulp
-
immature permanent teeth require apexogenesis for continued root development
Contraindications include pulp necrosis, advanced irreversible pulpitis with periapical pathology, or inability to achieve a proper coronal seal.
Treatment modalities
-
Indirect pulp capping: selective removal of infected dentin with protection of residual tissue with a cavity liner such as PD’s Cavity Liner light cure.
-
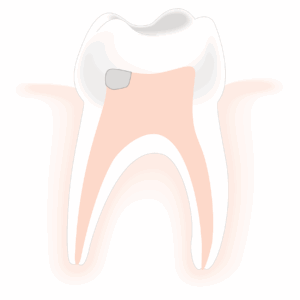
Direct pulp capping: application of a bioactive material over a small pulp exposure
-
Partial pulpotomy: removal of the superficial inflamed coronal pulp, preserving healthy tissue below
-
Full pulpotomy: removal of all coronal pulp while maintaining vitality of radicular pulp
Key prognostic factors
-
Strict isolation (rubber dam) to avoid contamination
-
Effective hemostasis: sodium hypochlorite (NaOCl) is widely recommended for pulp hemostasis and disinfection
-
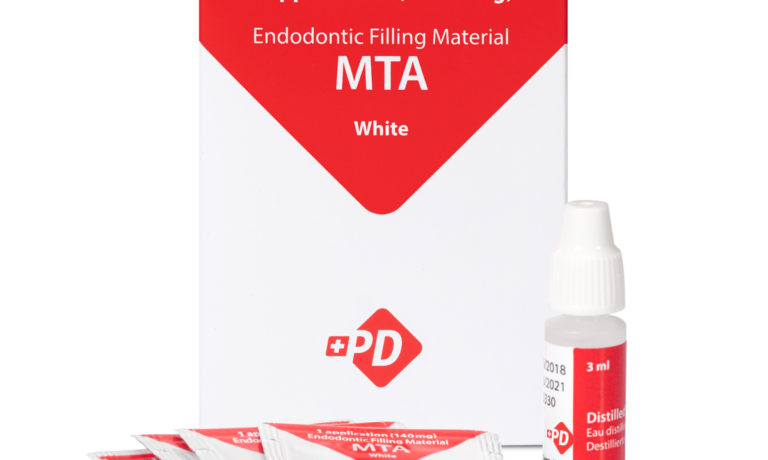
Choice of material: calcium silicate–based cements (MTA, bioceramics) provide superior biological and sealing properties compared to calcium hydroxide, with reported success rates of 85–100% in short-term studies
-
Immediate, definitive coronal restoration to prevent microleakage and support long-term outcomes
Clinical challenges and recent innovations
A common challenge in VPT is the precise and controlled placement of bioactive materials in a confined pulp chamber. Poor handling may compromise the coronal seal or disrupt pulp healing.
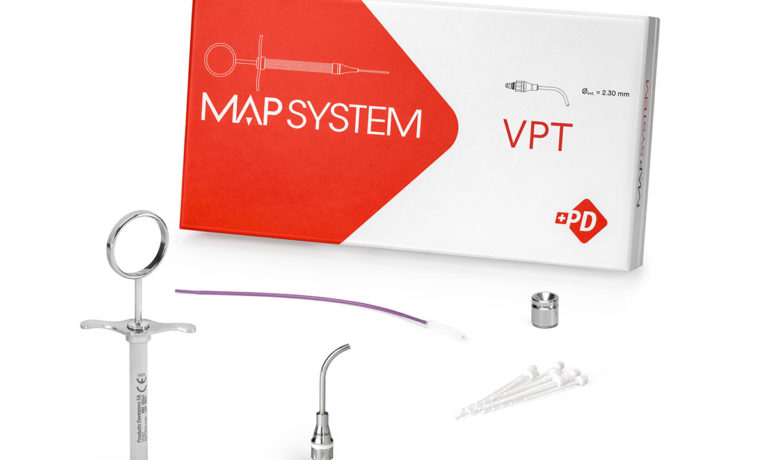
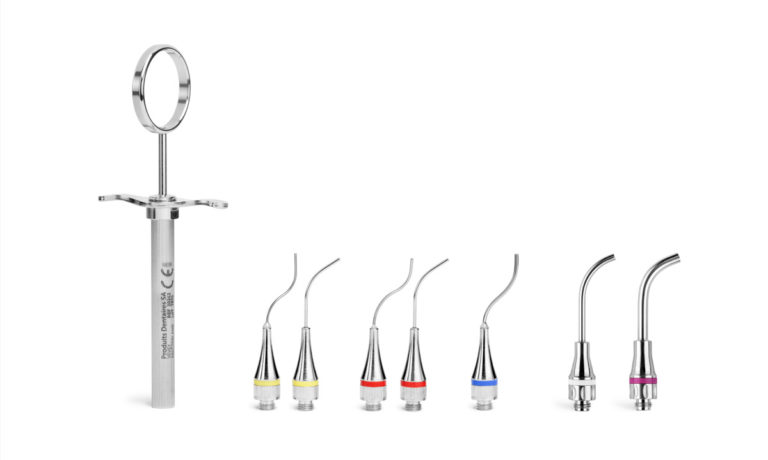
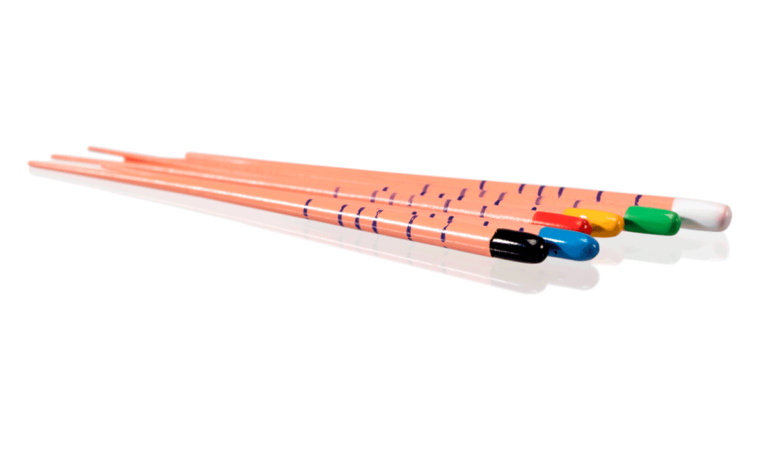
To address this, modern delivery systems have been developed. The MAP VPT system (Produits Dentaires, Switzerland) enhances precision during the placement of bioceramics in VPT procedures. It allows clinicians to:
-
deliver materials directly to the exposure site with accuracy
-
maintain visibility and control in restricted access
-
optimize the biological potential of pulp capping materials
Evidence and professional consensus
Numerous clinical trials and systematic reviews support VPT as a reliable option in both immature and mature permanent teeth. Importantly, the American Association of Endodontists (AAE) position statement (2021) affirms the effectiveness of VPT, extending its indications beyond immature teeth to include selected mature teeth traditionally considered candidates for root canal therapy. This reflects the growing consensus that VPT, when properly executed, is a biologically sound and predictable treatment.
Conclusion
Vital pulp therapy embodies the principles of modern endodontics: minimally invasive, biologically oriented, and focused on preserving natural tooth vitality. With appropriate diagnosis, bioactive materials, and precise placement techniques, VPT achieves high levels of clinical success.
Innovations such as the MAP VPT system integrate seamlessly into these protocols, supporting clinicians in delivering predictable outcomes while adhering to the biological principles outlined in current scientific evidence and professional guidelines.
References
- American Association of Endodontists. AAE position statement on vital pulp therapy. Chicago: AAE, 2021. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2021/05/VitalPulpTherapyPositionStatement_v2.pdf
- Chatterjee I, Agrawal P, Sinha Y, Majee N, Bansal S. In Vitro Response of Dental Pulp Stem Cells to Calcium Silicate-Based Cements: A Systematic Review and Meta-Analysis of Preclinical Evidence. Cureus. 2025 Jul 29;17(7):e88990. doi: 10.7759/cureus.88990. PMID: 40895876; PMCID: PMC12395108.
- Hatipoğlu Ö, Varlı Tekingür E, Pertek Hatipoğlu F. Comparative clinical success of direct pulp capping materials: A network meta-regression of randomized clinical trials. J Dent. 2025 Aug 29;162:106073. doi: 10.1016/j.jdent.2025.106073. Epub ahead of print. PMID: 40886932.
- Sharma R, Durga K, Wadhwa H. Vital Pulp Therapy for Traumatic Pulpal Exposure in Permanent Teeth: A Path to Healing? Insights From Existing Systematic Reviews. Dent Traumatol. 2025 Aug 28. doi: 10.1111/edt.70016. Epub ahead of print. PMID: 40874379.
- Valverde Haro HP, Erazo Conde AD. The Impact of Vital Pulp Therapy on Normal Root Development in Immature Teeth: A Case Report. Iran Endod J. 2025;20(1):e24. doi: 10.22037/iej.v20i1.47139. PMID: 40756760; PMCID: PMC12318324.
- Nagendrababu V, Nassar M, Govindaraju L, Kishen A, Abbott PV, Duncan HF. Teaching Vital Pulp Treatment for Permanent Teeth to Undergraduate/Pre-Doctoral Students: A Multinational Survey. Int Endod J. 2025 Aug 29. doi: 10.1111/iej.70020. Epub ahead of print. PMID: 40878810.